News & Events
News
What’s the Best Way to Reduce False Positives in Sterility Testing?
In order to release sterile medicines and products to the market, they must first pass a sterility test. How to help ensure sterility testing is a million-dollar question for every pharmaceutical firm. In this article, we break down which of the four common approaches is the most effective at reducing false positives. The stakes […]
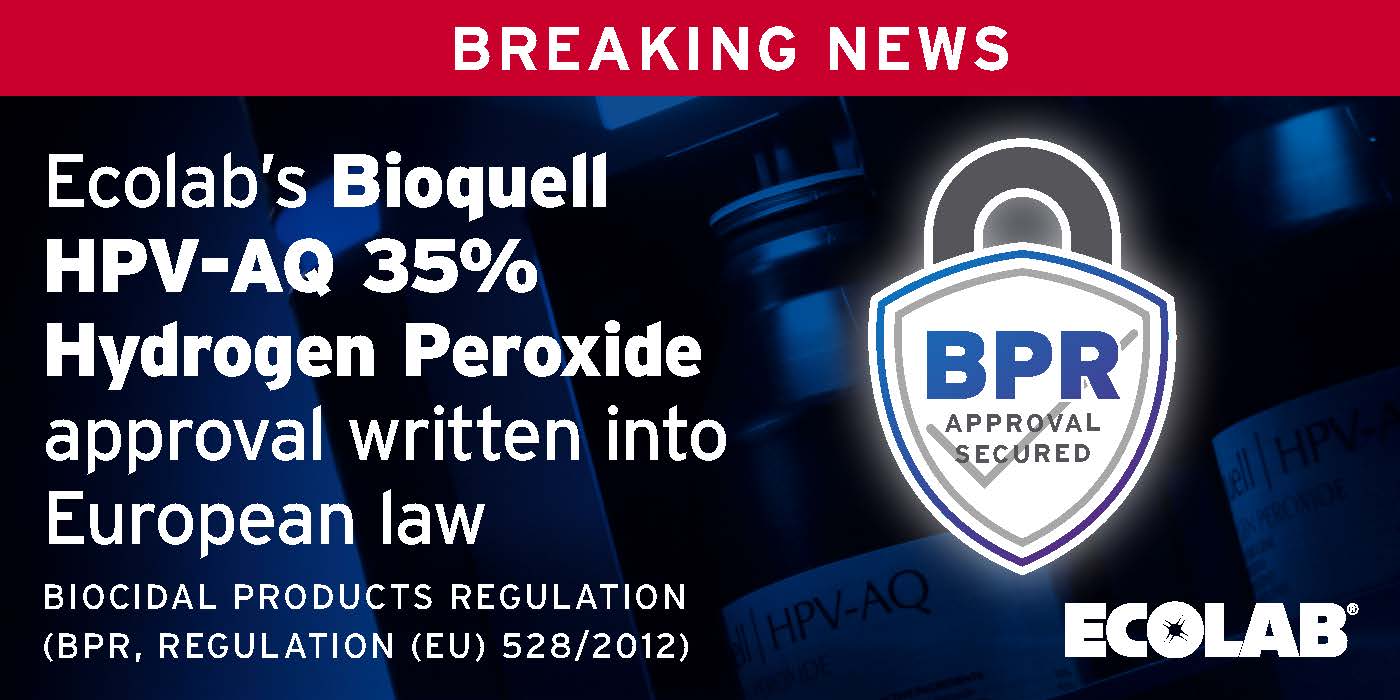
Read MoreEcolab’s Bioquell HPV-AQ 35% hydrogen peroxide approval written into European law
Earlier this year, Ecolab’s Bioquell HPV-AQ 35% hydrogen peroxide disinfectant received an approval opinion from the European Chemicals Agency (ECHA) Biocidal Products Committee (BPC) for a BPR EU (Union) Authorisation. We are pleased to communicate that the approval has been officially published in the Official Journal of the European Union and thus written into European […]
Read MoreSodexo Inc. – New Partnership with Ecolab to Help Reduce Hospital-Associated Infections
New Partnership with Ecolab to Help Reduce Hospital-Associated Infections Sodexo, world leader in food services and facilities management, announced an expanded partnership with Ecolab Inc., the global leader in water, hygiene and infection prevention solutions and services, to deliver a new infection prevention offering for hospitals and healthcare facilities across the United States. Sodexo’s unique […]
Read MoreHigher Hygiene Standards for Infection Control
In this Clinical Services Journal article, the topic of innovative decontamination efforts and hand hygiene tools are reviewed to show how they have helped hospitals raise infection control standards during the pandemic. Hospitals across the world saw cases rise while also dealing with unique challenges, whether PPE shortages, supply and staff issues, or finding effective […]
Read MoreFDA Authorizes Ecolab’s Bioquell Technology System for N95 Respirator Decontamination
FDA AUTHORIZES ECOLAB’S BIOQUELL TECHNOLOGY SYSTEM FOR N95 RESPIRATOR DECONTAMINATION Ecolab’s decontamination technology enables respirator reuse by healthcare personnel to help address shortages ST. PAUL, Minn. – December 18, 2020 – Ecolab Inc., the global leader in water, hygiene and infection prevention solutions and services that protect people and vital resources, has received Emergency Use […]
Read More